How Do Viruses Infect Cells The Science of Pathogens
Explore how viruses infect cells through the science of pathogens. Learn about viral entry mechanisms, replication cycles, and how the immune system responds to viral infections.
Viruses are microscopic pathogens that occupy a unique position in the biological realm, straddling the line between living and non-living entities. Composed of genetic material encased in a protein shell and, in many cases, a lipid envelope, viruses are notable for their ability to invade host cells and hijack their machinery for replication. Understanding the mechanisms through which viruses infect cells is critical for developing effective antiviral strategies and controlling viral diseases that impact public health globally. This field of study has gained increasing attention due to
The process of viral infection can be delineated into several stages: attachment, penetration, uncoating, replication, assembly, and release. Each stage is governed by intricate interactions between viral components and host cell receptors, dictating the specificity and efficiency of the infection. Controversies often arise regarding the extent of host immune evasion employed by certain viruses, as well as the implications of receptor variability on susceptibility and transmissibility. For instance, research into how genetic polymorphisms influence responses to infections, such as with HIV, underscores the complexity of host-pathogen interactions and the challenges posed by evolving viral strains.
Environmental factors, including habitat changes and climate dynamics, significantly influence viral transmission patterns and the emergence of zoonotic diseases, further complicating efforts to predict and manage viral outbreaks. As evidenced during the COVID-19 pandemic, public health responses must be adaptive, incorporating vaccination campaigns, hygiene practices, and educational initiatives to mitigate the impact of viral infections on communities. Consequently, understanding the science of viral infection is paramount in devising comprehensive approaches to protect global health and combat emerging infectious threats.
Structure of Viruses
Viruses are unique entities that exist at the boundary between living and non-living systems. They are characterized by their simple yet efficient structures, which enable them to invade host cells and exploit cellular machinery for replication. The funda- mental components of a virus include its genetic material, a protective protein shell, and, in some cases, a lipid envelope.
Types of Viruses
Viruses can be categorized based on their structure and presence of a lipid envelope. Viruses that lack an envelope are referred to as naked or non-enveloped viruses, while those that possess an envelope are termed enveloped viruses. The envelope is derived from the host cell membrane and is often studded with glycoproteins that facilitate recognition and binding to specific receptors on potential host cells[1][2].
This distinction significantly affects the mode of transmission and stability of viruses
Basic Components
At the core of each virus lies its genetic material, which can either be DNA or RNA. This genetic material is essential for the virus's replication and interaction with host cells. Encasing this genetic material is a protein coat known as the capsid. The capsid serves multiple functions: it protects the viral genome and aids in the virus's ability to attach to and penetrate host cells[3][4]. Capsids can exhibit various shapes and structures, such as helical and icosahedral forms, reflecting the virus's adaptability to different environments and hosts[5].
Viral Replication Process
The replication process of viruses begins with their entry into host cells. To infect a cell, a virus must first attach to a specific receptor on the cell's surface, similar to how a key fits into a lock. The surface proteins of the virus act as the key, initiating a process that allows the virus to either enter the cell as a whole or inject its genetic material into the host cell[6][5]. Once inside, the virus hijacks the host cell's machinery to produce new virus particles, enabling it to spread to additional host cells[3][4].
Mechanism of Infection
Viral infection occurs through a series of well-defined steps that allow viruses to invade host cells, replicate, and spread to new cells. This process can be broken down into six primary stages: attachment, penetration, uncoating, replication, assembly, and release[7][8].
Attachment
The initial step in viral infection is attachment, where a virus binds to a specific recep- tor site on the host cell membrane using attachment proteins present in the capsid or glycoproteins in the viral envelope. This interaction is crucial as it determines the specificity of the virus for particular host cells, akin to a key fitting into a lock[9][8]. For example, the rhinovirus utilizes its attachment protein to bind to the ICAM-1 receptor on human cells, facilitating its entry[10].
Penetration
Once attached, the virus penetrates the host cell. The mechanisms of entry vary among different types of viruses. Some, such as bacteriophages, inject their nucleic acid directly into the host cell through a syringe-like structure, while many animal and plant viruses may enter via endocytosis, wherein the cell membrane engulfs the virus[11]. Enveloped viruses can also enter through direct fusion of their membrane
Uncoating
After penetration, the virus undergoes uncoating, a process that involves the degra- dation of the viral capsid. This step releases the viral nucleic acid into the host cell's interior, where it can be utilized for replication and transcription[7][8].
Replication and Assembly
During the replication phase, the viral genetic material is incorporated into the host cell's machinery. This incorporation directs the host cell to synthesize viral
components, leading to the replication of the viral genome and the assembly of new virions[7][9]. Most DNA viruses typically replicate in the host cell's nucleus, while RNA viruses primarily replicate in the cytoplasm[8].
Release
The final stage of the viral life cycle is release, where new virions exit the host cell to infect adjacent cells. This can occur through two main mechanisms: budding or lysis. In budding, enveloped viruses acquire a portion of the host cell membrane as they exit, allowing the host cell to remain intact for a time[8]. Conversely, in lytic infections, the host cell is destroyed, releasing all new virions at once[7][9][8].
Understanding these mechanisms of infection is crucial for developing effective antiviral strategies and treatments to combat viral diseases.
Host Immune Response
The host immune response to viral infections is a complex and multifaceted process that involves both innate and adaptive immunity. Upon the entry of a virus int
Factors Influencing Virus Infection
Environmental Factors
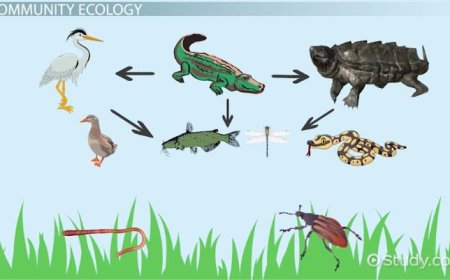
Environmental and ecological changes also affect viral infection dynamics. Factors such as habitat alteration, climate change, and increased host population density can facilitate viral transmission and potentially lead to new host interactions. For example, encroachment on wildlife habitats increases human-wildlife contact, cre- ating opportunities for zoonotic viruses to jump species barriers.[13] Understanding
Virus Entry Mechanisms
The process of viral infection begins with the entry of the virus into the host cell. This can occur through various mechanisms, including direct penetration, recep- tor-mediated endocytosis, and fusion with the cell membrane.[9] The effectiveness of these entry pathways is influenced by the infectivity of the virus, which refers
to the ratio of infective to defective viral particles. For example, viruses such as respiratory syncytial virus (RSV) typically require only a few viral particles to establish a productive infection, making them easier to study in imaging experiments compared to viruses with lower infectivity ratios, such as human immunodeficiency virus (HIV), which may require millions of particles to infect a single cell.[14]
Host Immune Response
The host immune system plays a critical role in determining the outcome of a viral infection. Pathogenic viruses are known to express gene products that help
them evade the host's antiviral defenses, including the production of interferons.[15] Humoral immunity, characterized by the production of antibodies, can neutralize viruses by blocking their attachment to host cells, but cannot eliminate the virus once it integrates its genome into the host's DNA. Cell-mediated immunity, involving cytotoxic T lymphocytes (CTLs), is crucial for recognizing and destroying infected cells, especially after viral replication has occurred.[15]
Receptor Variability
Variations in receptor expression among individuals and species significantly impact viral infectivity and transmissibility. Genetic polymorphisms, epigenetic modifications, and environmental factors contribute to this variability, which can influence how populations respond to viral threats. For instance, differences in the CCR5 receptor affect susceptibility to HIV infection, demonstrating how genetic diversity shapes host-pathogen interactions.[13] As viruses evolve to exploit new receptors, they can expand their host range, leading to potential cross-species transmission and public health challenges, as seen with zoonotic viruses like SARS-CoV-2.[13]
Pathogenicity and Viral Factors
The pathogenicity of a virus is also influenced by various viral factors, including the virulence of the infecting strain and the amount of viral particles released during infection.[15] These factors, combined with the immune status of the host and the presence of underlying health conditions, contribute to the disease's severity and outcome. Effective control measures, including vaccination and therapeutic inter- ventions, rely on a comprehensive understanding of these multifaceted interactions between the virus, the host, and environmental conditions.
Prevention and Treatment
Public health policies and individual actions are essential in preventing and treating viral infections. These efforts focus on reducing transmission rates and managing outbreaks through a combination of education, vaccination, and hygiene practices.
Vaccination
Vaccination is a key strategy in controlling the spread of viruses. Vaccines work by introducing a weakened or inactive form of a virus into the body, which stimulates an immune response. This response helps the body to recognize and combat the actual pathogen if encountered later[16][17]. Vaccination not only protects individuals but also contributes to herd immunity, making it more difficult for the virus to spread within the community. Widespread vaccination campaigns have significantly reduced the incidence of diseases such as polio and measles[17].
Public Health Campaigns
Public awareness campaigns are crucial in educating the population about preventive measures against viral infections. These campaigns emphasize the importance of proper hand hygiene, wearing masks, maintaining social distance, and practicing respiratory etiquette. By raising awareness, individuals are more likely to adopt these behaviors, leading to a decrease in transmission rates of infectious diseases[16].
Hygiene Practices
Practicing good hand hygiene is vital in reducing the risk of infection. Regular handwashing with soap and water effectively eliminates germs that may have been transferred from contaminated surfaces or people[16]. Additionally, following respira- tory etiquette—such as covering coughs and sneezes—further minimizes the risk of transmission.
Monitoring and Control
Effective public health policies involve monitoring and controlling outbreaks through surveillance systems and contact tracing. Surveillance systems help detect and track infections, allowing policymakers to identify trends and implement targeted inter- ventions to manage the infection rate[16]. Contact tracing ensures that individuals who may have been exposed to the virus are informed and can take necessary precautions, such as self-isolation or testing.
Challenges in Management
Despite these strategies, managing infection rates remains complex. Challenges include developing robust surveillance systems, ensuring timely reporting of cases, and sustaining vaccination efforts to maintain control over infection rates. A decline
References
[1] : Mechanisms of Viral Behavior and Host Interaction
[2] : Multiscale perspectives of virus entry via endocytosis
[3] : Multiplication of Viruses: Stages of Viral Replication - Embibe
[4] : Understanding Viruses: Structure, Transmission, and Vaccines
[5] : Understanding Viral Infection: Structure, Entry, and Spread
[6] : How do viruses get into the body? | Ask A Biologist
[7] : 15.5B: Steps of Virus Infections - Medicine LibreTexts
[8] : 5.7: Steps of Virus Infections - Biology LibreTexts
[9] : 21.2A: Steps of Virus Infections - Biology LibreTexts [10]: Viral replication - Wikipedia
[11] : Viral Entry, Immune Evasion, and Host Defense Mechanisms
[12] : Viral strategies for immune response evasion - Wikipedia
[13] : Viral Entry: Cell Receptors and Host Range Dynamics
[14] : Frontiers | Imaging Flow Cytometry and Confocal Immunofluorescence ...
[15] : REPLICATION IN VIRUSES – viral replication - Microbiology Class
[16] : Infection Rate vs Transmission Rate: What's the Difference?
[17] : Understanding Infection Rate: Explained
[undefined]: Frontiers | Uncovering Novel Viral Innate Immune Evasion Strategie